SPINAL DEFORMITIES
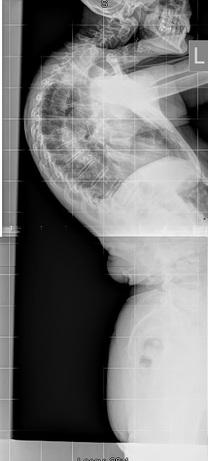
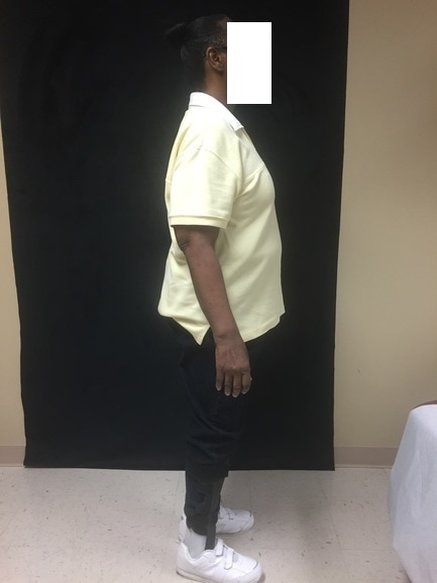
We specialize in a variety of surgical techniques used to treat spinal deformities. Spinal deformities can result in abnormal postures and cause back pain. Osteotomies or cuts in the bone are sometimes required to restore alignment
REVISION SPINE SURGERY
PROXIMAL JUNCTIONAL KYPHOSIS
Spine fusions place additional stress on the unfused portions of the spine. The level above the highest fused level can break down. In these circumstances, the spine may develop a sharp angulation at that junction known as proximal junction kyphosis. This can cause pain and deformity. Extending the fusion is necessary as shown below.
ADJACENT LEVEL DISEASE
Following spinal fusion, the levels that are unfused have to compensate for the motion that was provided by the previous fused segments. These levels that are unfused develop wear and tear and the disk at these levels degenerate at a higher rate. This can cause the bones to rub against one another or the disk to herniate causing pain. In these circumstances, we extend the fusion and may have to change the alignment of the spine in the process if the alignment from the original surgery is less than optimal.
INFECTIONS
Infections can be devastating and can lead to pain and disability. Usually, patients can be treated with intravenous antibiotics. Certain infections can cause deformities and the infection may be so severe that it can compression on the spinal cord and require surgery to decompress the spine and correct any deformities present.
SPINAL TUMORS
METASTATIC SPINAL CORD COMPRESSION
Metastatic spinal cord compression can lead to severe back pain and loss of neurological function. Recent randomized controlled trials by Patchell et al., Lancet 2005 suggest that surgery has a defined role and is superior to radiation in terms of maintaining neurological function and preserving quality of life in individuals diagnosed with metastatic tumors that are not radiosensitive. Recent advances have allowed surgeons to treat metastatic tumors of the spine, sometimes without the need of a surgery through the chest. The goals for surgical intervention in dealing with metastatic tumors is to 1) decompress the spinal cord and 2) stabilize the spine.
PRIMARY SPINAL TUMORS
Spinal tumors arise from tissue present within the spinal cord or nerve roots or the cells or tissues that surround or support the function of the spinal cord or nerve roots. Primary spinal cord tumors can be benign (or non-cancerous). In these circumstances, a resection of tumor can preserve neurological function and lead to a cure.
SPINAL FRACTURES
CERVICAL NECK FRACTURES
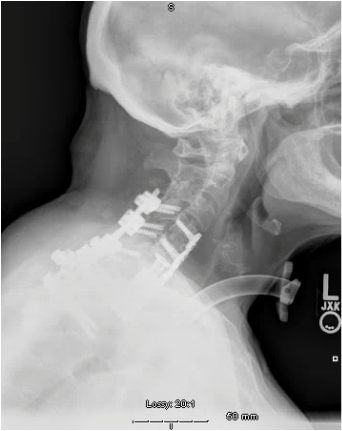
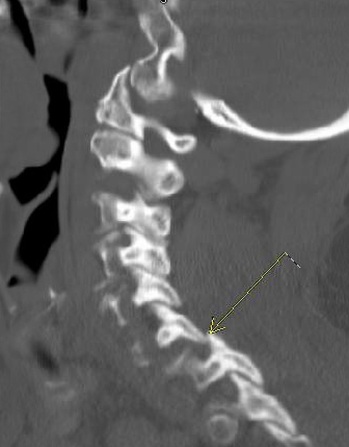
Cervical neck fractures can lead to instability of the cervical spine placing an individual at risk for paralysis. Some fractures can be treated conservatively with a hard collar but there are some fractures that can develop instability unless surgically treated. Two common types of fractures that we treat surgically in the cervical spine are 1) jumped/perched facets and 2) odontoid fracture. Jumped facets occur when the joints in the spine slip and get locked in an abnormal configuration as shown below. Surgery requires aligning the spine and fusing the two segments together.
Cervical neck fractures can lead to instability of the cervical spine placing an individual at risk for paralysis. Some fractures can be treated conservatively with a hard collar but there are some fractures that can develop instability unless surgically treated. Two common types of fractures that we treat surgically in the cervical spine are 1) jumped/perched facets and 2) odontoid fracture. Jumped facets occur when the joints in the spine slip and get locked in an abnormal configuration as shown below. Surgery requires aligning the spine and fusing the two segments together.
Cervical neck fractures can lead to deformities and cause debilitating pain as well as potential paralysis. Fusion is necessary to stabilize the spine but sometime it is necessary to correct the malalignment in the process. In the cervical spine, applying a method called cervical traction where a pulley system is used to provide distraction on the head can reduce the abnormal curvature before the spine is fixated by screws and rods.
Odontoid fracture are fractures occurring in C2. They have a lower chance of healing than fractures in the remainder of the cervical spine. In these circumstances, we take into consideration the age of the patient, whether the fracture is aligned, and whether there are any risk fractures that may prevent healing of the fracture. Non-healing fractures that are unstable and move with flexion-extension movements of the neck can be treated surgically with a posterior cervical fusion as shown below.
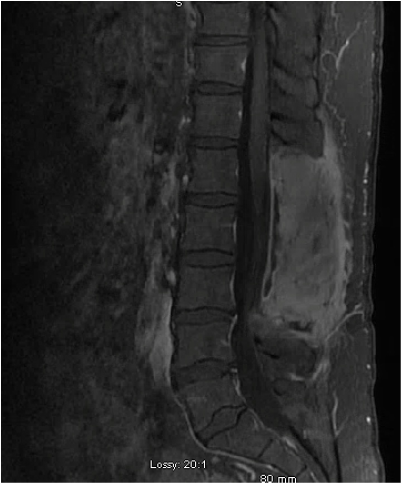
THORACOLUMBAR FRACTURES
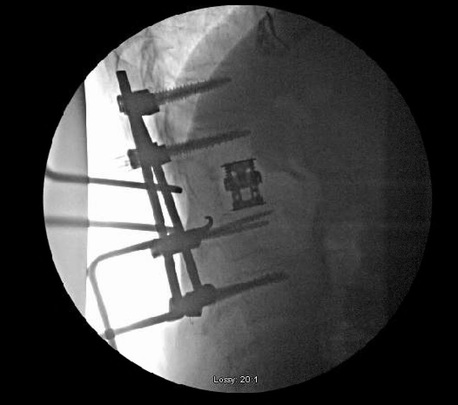
Like cervical fractures, typically, these fractures can be treated conservatively with bracing. However, in rare circumstances where there is fragments of bone causing compression of the spinal cord or angulation resulting from the fractures, surgery can be an option. The treatment of the fracture can be done with surgery through one incision through the back.
For example, we have treated a 55 year old female who fell. Following the accident, she started developing weakness in the legs as well as severe pain in the back. She was diagnosed with a T12 burst fracture. Her fracture had bone that had migrated into the canal causing compression of the spinal cord. There was a mild focal angulation in the region of the spine. As a result, she underwent a fusion at from T10 to L2 and the fracture segment was removed and replaced with a metallic cage.
DEGENERATIVE SPINAL CONDITIONS
CERVICAL DEGENRATIVE CONDITIONS
Cervical degenerative conditions can cause impingement of the spinal cord or the nerve roots. When the spinal cord is being pinched by herniated disk or thickened ligaments, the patient can experience 1) difficulty walking 2) weakness in the hands or legs 3) difficulty buttoning clothes 4) worsening handwriting 5) stiffness in the arms and legs and/or 6) pain in the neck and shoulder. When the spinal cord is affected, there can be permanent loss of neurological function and the longer the condition goes untreated, the less likely the patient will recover.
On the converse, symptoms related to a herniated disk causing impingement on the nerve roots and NOT the spinal cord can lead to weakness in a particular muscle group or pain and numbess in a particular region that is supplied by the nerve root. If pain and numbness are the main symptoms, conservative management with physical therapy and epidural steroid injections is appropriate. However, when weakness comes into play, surgery is a better option. There are multiple procedures to treat these conditions:
Laminectomy
Laminectomy and posterior fusion
Anterior cervical discectomy and fusion
Anterior cervical disk replacement
Laminoplasty
Although some surgeons may feel accustomed to routinely performing one or two of these procedures, it is best if you understand why the others options are not good options when discussing the best surgery for your condition.
LUMBAR DEGENERATIVE CONDITIONS
Degenerative conditions of the lumbar spine can produce leg and/or back pain. In these circumstances, we evaluate whether there is any impingement on the nerves from bone spurs, herniated disk, and thickened arthritic joints or ligaments. When there is nerve compression, patients classically present with leg pain. As the disk and joints degenerate, the alignment of the lumbar spine can be thrown off and there can be rubbing of the bone on one another causing back pain. Thus, our goals of surgery are to relieve unwanted symptoms. A procedure done to remove bone or disk to relieve pressure on the nerves is relatively small and can most times be done minimally invasive through small tubes through an incision length the size of a penny.
In most cases a procedure done to relieve pressure on the nerves does not alter the mechanics of the spine much. If a fusion is required, there can be significantly more surgical planning that goes on before the operation to optimize benefit and prevent unwanted complications. Typically, back fusions are reserved when the spine is unstable (when the vertebrae moves significantly in relation to one another) or back pain is a significant component and felt to be related to degenerative disk disease. Planning for a fusion requires more than just understanding the most obvious problem where the disk is degenerated. It is important to take into account the overall alignment of the spine before fusing the spine to prevent an unfavorable alignment where a patient can have difficulties stand standing up after the operation. Bad outcomes can result from surgeries if patients have: 1) Poor alignment after an operation 2) The levels above and below the fusion begin to degenerate 3) The bones never fuse (fusion of the bone can take up to one year) and/or 4) There is a spinal infection. Minimally invasive techniques can be employed for lumbar spinal fusions as well.